Mental health awareness campaigns are more prevalent than ever, yet the concept itself remains misunderstood, overlooked, and stigmatized – even by the experts. Recognizing this, Dhwani and The Red Door organised ‘Vivridh’, a space for open conversations about mental health. The symposium was held in memory of a student at Dhwani who ended her life last year. Diagnosed with Borderline Personality Disorder, her story became a call to reflect on how we, as a society, can better support those around us. The event opened with a moving short film on her life, leaving the audience with moistened eyes and deep questions- if medicine alone could fix mental illness, why is she not here with us today?
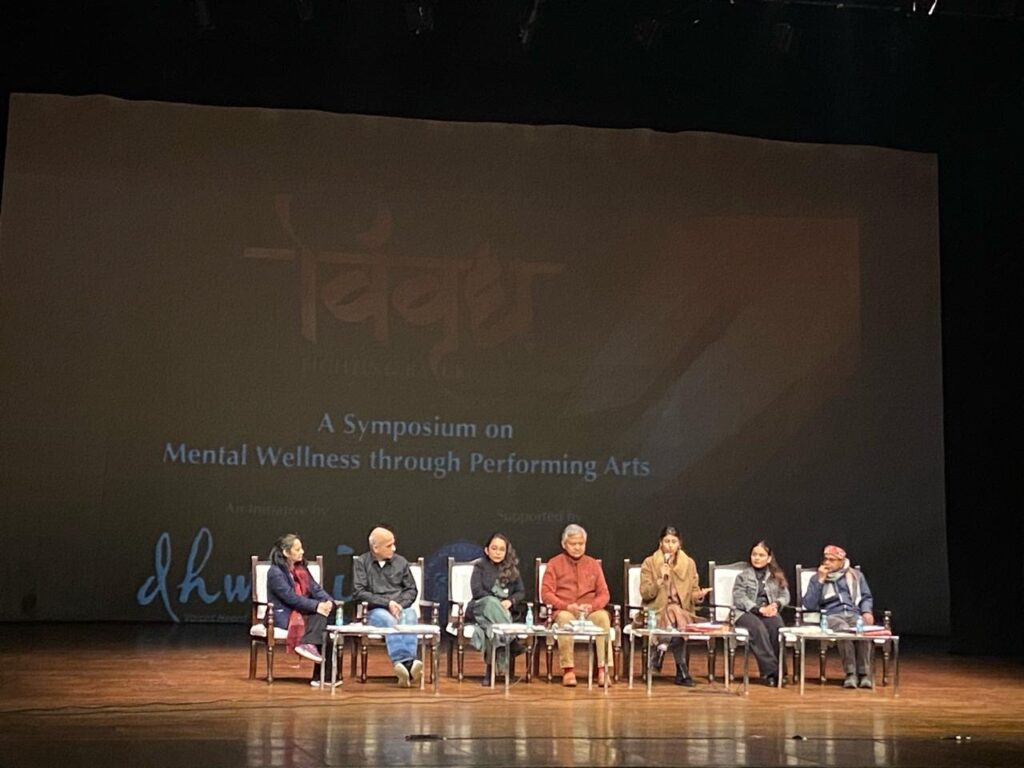
A panel discussion followed which was moderated by Aparna Sanyal of The Red Door. It addressed the thoughts stirred by the film included key stakeholders from the mental health system, each bringing unique insights.
Surviving Psychiatry: Pranami Tamuli’s Story
First on the panel, Pranami Tamuli, Executive Director of the The Red Door, started by sharing her lived experience with the mental health system.
She explained how mental health struggles are often misunderstood and misdiagnosed, which can negatively impact individuals. However, when she met someone who linked mental health to life experiences rather than just medical conditions, her perspective shifted. She realized that healing goes beyond medication and diagnosis.
“If we were to look at these mental health issues are functional responses to things that are going on in our life rather than chemical imbalances” she said.
Her experience highlighted how mental health issues are often pathologized without understanding the underlying emotional and social contexts. Her story showed that mental health is more than just labels. It’s about being understood, supported, and given space to heal. You do not have to be a trained mental health expert to understand human struggles and make lives better; you can do it by being a kind and compassionate human being too.
Psychiatric Expert: Amit Sen’s Journey of Unlearning

Next, renowned psychiatrist Dr. Amit Sen shared his insights. He spent the first ten years of his career learning about mental illness diagnoses and treatments but spent the next 25 years “unlearning them and getting closer to real human experiences” he said. Unlearning allows professionals to move beyond the rigid medical labels and see the full complexity of mental health. By shifting focus from just diagnoses and prescriptions to real human experiences, they can better understand the emotional, social, and environmental factors affecting a person’s well-being. This approach leads to more compassionate care, where people feel heard and supported rather than just treated as a set of symptoms. It also challenges the idea that medication alone is the solution, encouraging holistic healing that includes therapy, social support, and life changes.
He critically analysed the overdependence on the biomedical model that views mental health issues as medical conditions caused by biological factors like brain chemistry or genetics. It focuses on diagnosis and treatment with medication or therapy. This approach tends to ignore the complex ways in which a person’s emotions, social interactions, and living conditions affect their mental health. For example, someone experiencing anxiety or depression may not only be struggling because of brain chemistry or genetics but also due to factors like stress from work, family problems, loneliness, financial struggles, or past traumatic experiences.
Mental health, like physical health, is shaped by multiple factors—poverty, trauma, marginalization, learning disabilities, and social pressures. Yet, society often shifts responsibility onto individuals, expecting them to “fix” themselves with medication while ignoring the environments that contribute to their struggles.
Alternative psychiatry: Aditya Tiwari’s Homeopathic Approach
Next, homeopathic psychiatrist Dr. Aditya Tiwary, highlighted the deep connection between society and mental well-being.
“What happens in the symptoms approach or the diagnosis approach, we are trying to disperse off the smoke that we see. We are not attempting to address where the fire is coming from” he said.
True healing, he explained, comes from understanding individuals, and not just their diagnosis. Instead of just focusing on symptoms and medical terms, it’s essential to understand the individual—their personal experiences, emotions, struggles, and the unique circumstances that shape their mental health.
He warned that in today’s world, there is a growing tendency to overlook a person’s subjectivity—their own thoughts, feelings, and perspectives. People are often told how they should feel based on medical definitions or societal expectations, rather than being given the space to express what they actually feel.
Centring Lived Experience: MISA’s Ayurdhi Dhar Talks About Context
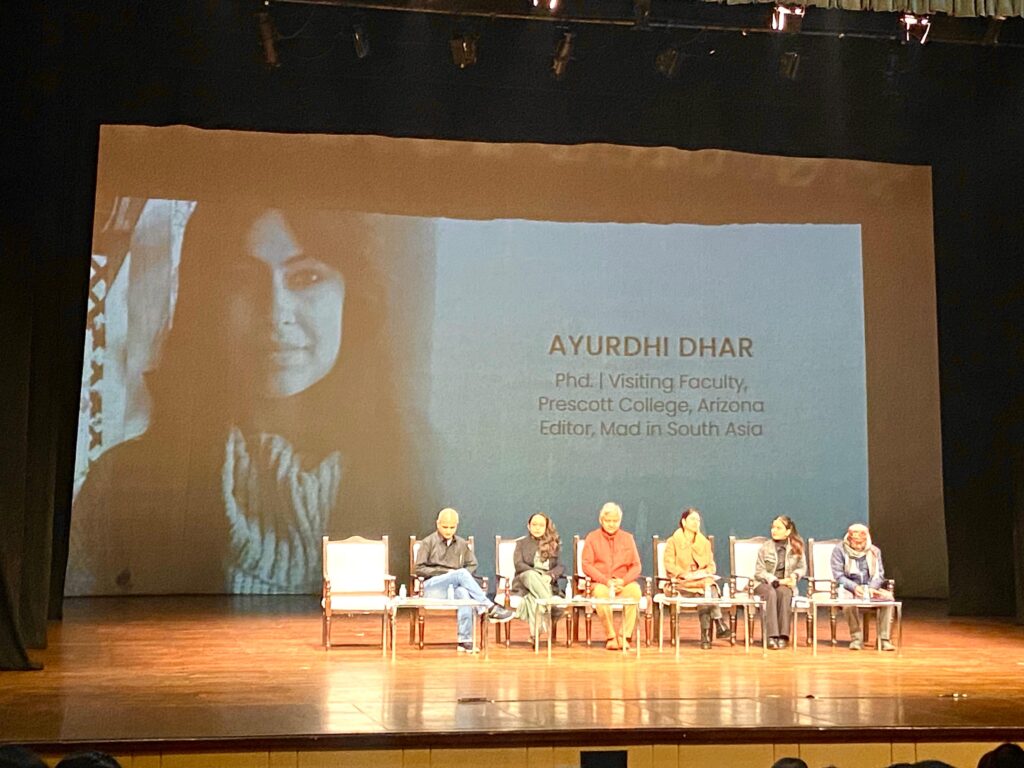
Next in conversation was our Editor, Dr Ayurdhi Dhar. Dhar re-emphasized the importance of listening to the stories of people with lived experiences with the mental health system. People who have personally experienced mental health challenges and navigated mental health systems (such as therapy, medication, or institutional care) have first-hand knowledge of what really helps and what does not. Their insights are valuable because they provide real-world perspectives that may vary from theoretical approaches or medical models. This is where the gap in the psy disciplines lies, she added. It often focuses too much on the medical model and ignores personal and social contexts, which can harm people rather than help them.
Dhar made her case by sharing a story shared with her by the resilience expert, Micheal Ungar highlighting a case of a young boy diagnosed with Oppositional Defiant Disorder (ODD). The real issue, however, was not within the child but in the external world—his father had to relocate for work due to fluctuating oil prices, reducing the family’s income. This disrupted the child’s routine, friendships, and sports activities, which caused distress. His behaviour was labelled as a disorder when, in reality, it was a response to life changes.
She argued that Psychology often looks only at the individual and ignores bigger issues like poverty, discrimination, and social isolation, which all affect mental health. Often these theories about human behaviour stem from the Western societies, college students, and White participants. Generalising this to the whole world has many potential risks involved. Through her talk, Dhar encouraged a shift in perspective- moving away from purely medicalized understandings of mental health and toward a broader, more contextualized approach.
Expert by Experience: Alee’s Chosen Path to Healing
Alee, an expert by experience, was someone who had personally navigated mental health struggles and found her own ways of healing. She shared her journey of coping with loss and grief. As a college student, Alee’s struggle with the high cost of mental health treatment is a reality still shared by millions across the world. Many people, especially students and those with low incomes, cannot afford therapy, doctor visits, or medicine for mental health. Because of this, they often struggle alone, depend on weak support systems, or turn to other options that may not be helpful.
This lack of access to mental health care is a big problem. Her story highlighted the lack of access to professional care and the need for more affordable mental health solutions. Through dance, Eastern wisdom, and self-exploration, she found ways to regain control over her well-being.
Socializing Mental Health: Suicide as a Failure of Society
With Snehi having helped over 1,58,000 people in crisis and trained 1,580 individuals, Mr Mabood emphasized the importance of a community-driven approach to mental health.
“Suicide speaks as much about the pathology of the society as it does about the psychology of the individual” he said, echoing many psychologists from Erich Fromm to Ken Gergen.
This highlights that suicide is not just a personal or psychological issue but also a reflection of deeper societal problems. While mental health struggles play a role, social factors like poverty, discrimination, loneliness, academic or workplace pressure, and lack of emotional support often contribute to a person’s distress.
In many cases, individuals who die by suicide are not just suffering from mental health challenges but also from isolation, hopelessness, and the feeling that they have no way out. If a society places extreme pressure on success, ignores mental health, or fails to provide strong support systems, it creates an environment where vulnerable individuals feel trapped. If we want to prevent suicide, we must address both individual mental health care and the social conditions that contribute to despair. We as members of the society need to take responsibility of mental health of people around us.
He also pointed out a major issue among young people today—loneliness. “nowadays, people are chatting and not talking”. There is a need to address this lack of social ties in a society known for its strong social bonds.
Instead of seeking real human connection, people are buying things they do not need, filling their houses and life with commodities, standing for hours in front of their wardrobes, unable to decide what clothes to wear, he added. Psychologist, Philip Cushman, explains this through the idea of the “empty self” (Cushman, 1990), where individuals, feeling a sense of inner emptiness or lack of purpose, seek fulfilment through external means—food, consumer products, social media validation, or idolizing celebrities. Instead of addressing deeper emotional or societal issues, people attempt to “fill” this void with material possessions or curated identities.
At Vividh, Abdul emphasized that mental health cannot be reduced to just individual diagnoses; it is deeply linked to societal structures. The pressure to constantly consume—whether products, social media content, or external validation—prevents people from truly connecting with themselves and others. He urged for a shift from pathologizing mental health to socializing it, where healing comes from meaningful relationships, open conversations, and a sense of community rather than material distractions.
A common theme in all these discussions was the need to create a better space for people experiencing mental health challenges to breathe, live, and heal.
Medication and therapy alone are not enough. Society plays a key role in the healing process. If people were more sensitive to the needs of those struggling with mental health issues—whether diagnosed or not—we could prevent so many crises. Change does not have to be brought by someone else but ourselves- look out for people in your family, friends circle, schools/colleges/workplaces, neighbourhood or just on the streets or while strolling in the park. Some assurance that it is okay to feel a few things can save millions of life.
Key takeaways for the audience-
- Mental health is shaped by life experiences, not just medical labels.
- Mental health is a social responsibility.
- Mental health is not individual but often rooted in social issues like poverty, discrimination, abuse, and social pressures.
Through performances, discussions, and personal narratives, Vividh created a space to talk about mental health openly, break the stigma, and emphasize the need for a more compassionate and community-driven approach to well-being.
Ayushi Jolly
Ayushi Jolly is a PhD Scholar in Social Psychology at Jawaharlal Nehru University. Her research interests include Critical, Social, Indigenous, and Cultural Psychologies. Her research focuses on moving beyond individual focused explanations to understanding the self as embedded in dynamic social contexts.
Outside the academic sphere, she relishes the joy of travel and trekking and finds solace in mountains and the world of non-fiction.

